Proton Beam Therapy
Precision with less side effects
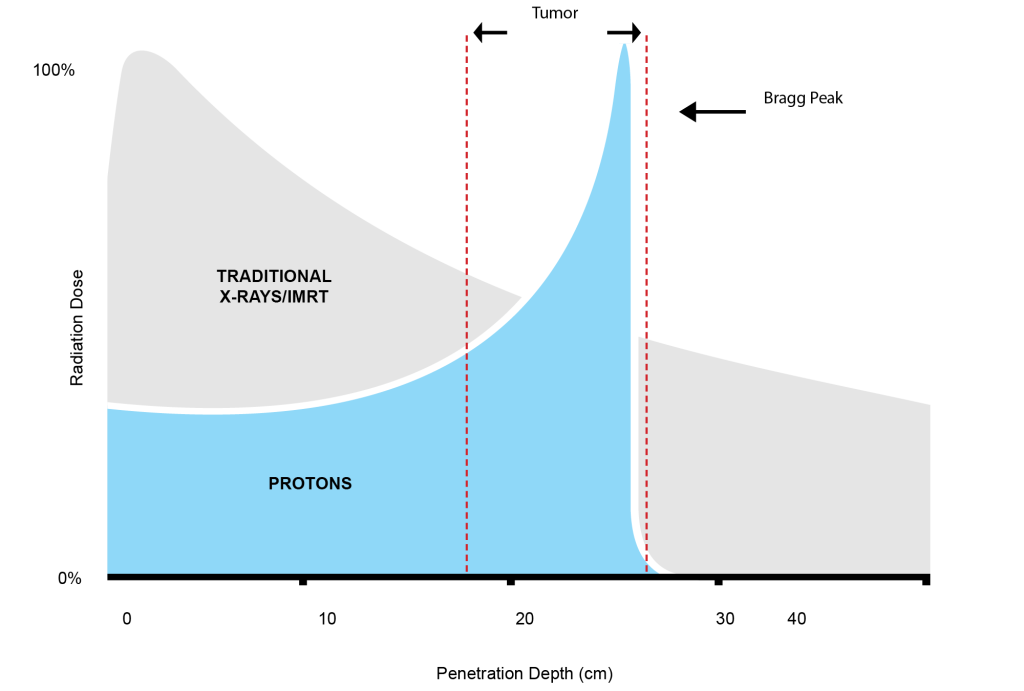
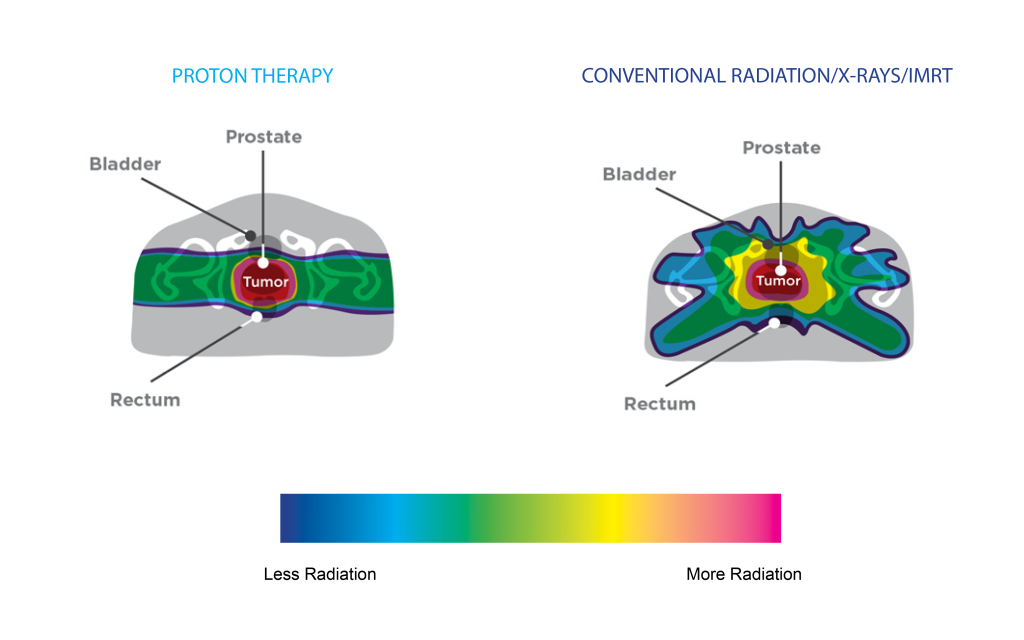
Proton therapy is an advanced form of radiation therapy that utilizes protons, charged particles, to target and treat tumors with remarkable precision. Unlike traditional radiation therapy, which uses X-rays and can pass through healthy tissues beyond the tumor, proton therapy exploits the ‘Bragg Peak’ phenomenon. As protons travel through the body, they release their energy at a specific depth, creating this peak of radiation dose. This ensures that the maximum radiation is delivered directly to the tumor while minimizing exposure to surrounding healthy tissues. Proton therapy is an effective option for treating many different types of cancer.
I went from being the doctor to the patient.
- James Gray, M.D., Medical Director
Dr. James Gray, a distinguished Radiation Oncologist with over three decades of experience, suddenly found himself in a patient’s shoes in 2019. Initially seeking care for a minor health issue, an elevated PSA level screening led to a prostate cancer diagnosis. While he had guided countless patients through such moments, now he was the one grappling with the emotions and decisions.
Despite the personal challenge, his professional expertise guided him confidently to a decision: proton therapy. Cognizant of its benefits, especially in minimizing radiation to surrounding tissues, Dr. Gray said, “I know what I consider to be the best treatment for prostate cancer and that is proton therapy.” His dual role as both doctor and patient underscores his faith in the treatment and the exceptional care at the Tennessee Oncology Proton Center.
At the Tennessee Oncology Proton Center, our patients experience the gold standard of precision with Pencil Beam Scanning proton therapy.
Pencil Beam Scanning, as its name suggests, employs a razor-thin beam to deposit protons directly onto the tumor. This technique unfolds layer by precise layer, much like masterful strokes from an ultra-fine brush, ensuring that cancerous cells are targeted with unmatched accuracy, while the surrounding healthy tissue remains unharmed.
Precision and Accuracy
PBS allows for a highly precise delivery of proton radiation, targeting tumors layer by layer, often to within a millimeter. This accuracy is especially crucial for tumors that are irregularly shaped or located near critical structures in the body.
Intensity Modulation
PBS can modulate the intensity of the proton beam, allowing for a variable radiation dose to be delivered across the treatment area. This intensity modulation ensures that the entire tumor receives the prescribed dose while minimizing exposure to surrounding healthy tissues. We call this Intensity Modulated Proton Therapy, or IMPT.
Minimized Radiation Exposure
Due to its precision, PBS reduces the risk of radiation exposure to surrounding healthy tissues and organs. This can lead to fewer short-term side effects and lowers the long-term risk of secondary cancers compared to traditional radiation therapy techniques.
Advances Over Passive Scatter
Compared to passive scatter proton therapy, Pencil Beam Scanning offers a more refined delivery of radiation. While passive scatter spreads the proton beam out over the target area, PBS paints the tumor point by point and layer by layer. This distinct method allows for even greater precision, especially for complex tumor shapes and when tumors are adjacent to sensitive structures. The result is potentially fewer side effects and even more precise targeting of the tumor.
Proton Therapy vs. Traditional Radiation
Both proton therapy and traditional X-ray radiation serve the same purpose in oncology: to impede cancer cells from multiplying and expanding. The distinction lies in how they administer their treatment. Protons, being subatomic particles, can be precisely directed to release radiation at specific depths, focusing most of their energy right on the tumor, then ceasing.
Conversely, traditional X-ray radiation beams emit radiation from their entry point on the skin, continuing beyond the tumor. This means healthy cells in the trajectory of the X-ray beam can be affected, raising the risk of harm to adjacent tissues and organs.