Estimated Reading Time: 7 minutes
Key Takeaways
- A dosimetrist is a vital healthcare professional who specializes in planning and calculating radiation doses for cancer treatment.
- They utilize advanced imaging (CT, MRI, PET) and specialized software to create precise, individualized 3D treatment plans.
- The core objective is to deliver the maximum effective radiation dose to the tumor while minimizing exposure to surrounding healthy tissues and organs.
- Dosimetrists collaborate closely within a multidisciplinary team, including radiation oncologists, medical physicists, and radiation therapists.
- Becoming a dosimetrist requires significant education: typically a bachelor’s degree followed by specialized training in medical dosimetry and often certification (CMD).
- They differ from radiation therapists, who are responsible for the daily delivery of the planned radiation treatment.
- Accurate dosimetry is critical for optimizing treatment effectiveness, ensuring patient safety, and reducing potential side effects.
Table of Contents
A dosimetrist is a highly skilled healthcare professional who specializes in the precise planning and calculation of radiation doses used in cancer treatment. Understanding what a dosimetrist is, is key to appreciating the complexity and care involved in modern radiation therapy. These experts play a critical role of a dosimetrist in cancer treatment. They are essential members of the radiation oncology team. (Get familiar with your Clinical Team). Their work ensures that radiation, a powerful tool against cancer, is delivered safely and effectively.
The field of medical dosimetry involves creating detailed treatment plans that target cancerous tumours while carefully avoiding damage to surrounding healthy tissues. This precision is especially vital in advanced treatments like proton therapy (learn what to expect with proton therapy), where the radiation beam can be controlled very accurately. Dosimetrists work behind the scenes, using their knowledge of physics, anatomy, and technology to design the best possible plan for each patient. Their contribution is crucial for patient safety and achieving the best possible treatment results. Understanding their role helps patients and other healthcare providers recognize the detailed planning that goes into every radiation treatment.
Research confirms that a dosimetrist ensures the accurate delivery of radiation doses to treat cancer while minimizing harm to healthy tissues. (See insights from Trusted Health) Their expertise is particularly significant in advanced treatments like proton therapy. (Discover more via Sharp Health News).
What is a Dosimetrist: Definition and Skills
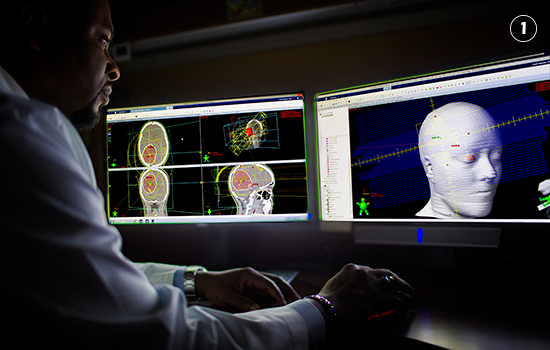
So, what is a dosimetrist? They are medical specialists who design and calculate radiation treatment plans tailored specifically for each cancer patient. Think of them as the architects of radiation therapy. Using advanced computer software and imaging scans like Computed Tomography (CT), Magnetic Resonance Imaging (MRI), or Positron Emission Tomography (PET), they create precise three-dimensional (3D) models of the patient’s body. These models show the exact location and shape of the tumour, as well as nearby healthy organs and tissues that need to be protected.
Their primary job within medical dosimetry is to figure out the exact dose of radiation needed to destroy the cancer cells and the best way to deliver that dose. This involves complex calculations and simulations to ensure the radiation beam targets the tumour shape accurately from the right angles and intensities. They work closely with the radiation oncologist, who prescribes the total radiation dose, to develop a plan that meets the doctor’s goals. The dosimetrist’s plan guides the radiation therapists who actually deliver the treatment.
Dosimetrists leverage imaging modalities like CT, MRI, or PET scans to create 3D models of the patient’s anatomy and accurately plan radiation delivery. (Learn more here) They are essential members of the radiation oncology team, specializing in precise planning and administration of radiation therapy. (Read the overview by the American Association of Medical Dosimetrists).
Becoming a dosimetrist requires significant education and training. Most start with a bachelor’s degree, often in a science field like physics, mathematics, or sometimes radiation therapy. After their bachelor’s degree, they must complete a specialized training program in medical dosimetry. These programs are typically 12 to 24 months long and must be accredited by the Joint Review Committee on Education in Radiologic Technology (JRCERT). The curriculum covers topics like radiation physics, radiobiology (how radiation affects living tissues), anatomy, treatment planning techniques, and computer skills.
Upon completing their education, most dosimetrists seek certification from the Medical Dosimetrist Certification Board (MDCB). While not always legally required, certification is highly preferred by employers and demonstrates a high level of competence in the field. To become certified, candidates must pass a rigorous exam that tests their knowledge and skills in dose calculations, treatment planning, radiation safety, and quality assurance. Maintaining certification often requires ongoing education to stay current with the latest advancements in medical dosimetry.
To become a dosimetrist, individuals typically need a bachelor’s degree followed by specialized training in medical dosimetry. (Explore education paths at HealthcareDegree.com) Certification ensures proficiency in treatment planning, dose calculations, and radiation safety. (Find career details on Indeed).
Dosimetrists usually work in the radiation oncology departments of hospitals or dedicated cancer treatment centers (take a virtual tour of a proton therapy center). Some may also work in research facilities or for companies that develop treatment planning software or radiation delivery equipment. They are key members of a multidisciplinary cancer care team. This team approach is central to the role of a dosimetrist in cancer treatment. They collaborate daily with radiation oncologists (doctors specializing in radiation therapy), medical physicists (experts in radiation physics and equipment), and radiation therapists (technologists who operate the treatment machines and administer the radiation). This teamwork ensures that the intricate treatment plans are developed safely and implemented correctly for each patient.
Dosimetrists work alongside oncologists, medical physicists, and radiation therapists. (Learn about the allied health career via Trusted Health) They are integral in both clinical and research settings. (Understand their scope from the American Association of Medical Dosimetrists).
The Crucial Role of a Dosimetrist in Cancer Treatment
The primary role of a dosimetrist in cancer treatment centers around meticulous treatment planning. They are the main professionals responsible for designing how radiation will be delivered to a patient. This involves taking the radiation oncologist’s prescription—which specifies the total dose of radiation needed—and creating a detailed, step-by-step plan to achieve it. Using specialized computer software, the treatment planning dosimetrist calculates the precise dose distribution. This means figuring out how much radiation will reach the tumour and how much will affect surrounding healthy tissues.
Their goal is always twofold: deliver a high enough dose to effectively control or eliminate the cancer, while keeping the dose to nearby critical organs and healthy tissues as low as possible. This careful balancing act is a core part of medical dosimetry. They simulate different beam arrangements, angles, and intensities to find the optimal approach for each unique patient situation. The complexity of this task requires a deep understanding of physics, anatomy, and the technology being used. The final treatment plan includes detailed instructions for the radiation therapists who will administer the treatment sessions.
Dosimetrists ensure the prescribed radiation dose is delivered precisely to the tumor while protecting nearby healthy tissues. (Read about precision at Ironwood Cancer & Research Centers) Their goal is to achieve maximum tumor control while minimizing side effects. (See the focus at Ironwood Women’s Centers).
Effective cancer care relies heavily on teamwork, and the role of a dosimetrist in cancer treatment necessitates close collaboration with other members of the radiation oncology team. They work directly with the radiation oncologist to understand the treatment goals and any specific concerns for the patient. They also collaborate closely with medical physicists who are responsible for the calibration and quality assurance of the treatment machines and planning systems. This ensures the equipment performs exactly as expected according to the dosimetrist’s plan.
Furthermore, dosimetrists communicate constantly with the radiation therapists who deliver the daily treatments. If any issues arise during treatment or if adjustments to the plan are needed based on patient changes or new imaging, the dosimetrist works with the team to modify the plan accordingly. This ongoing communication loop between the dosimetrist, oncologist, physicist, and therapist is essential for ensuring the treatment is delivered safely and accurately throughout the entire course of therapy.
Their work requires close coordination with oncologists and therapists to achieve optimal patient outcomes. (Watch a Medical Dosimetrist Overview on YouTube) Dosimetrists are vital for implementing advanced treatment plans. (Learn why from the American Association of Medical Dosimetrists).
While much of their work happens behind the scenes, the role of a dosimetrist in cancer treatment also extends to aspects of patient care and education. Although radiation therapists have more direct daily contact with patients during treatment delivery, dosimetrists often participate in the initial simulation process where imaging scans are taken for planning. They may also be involved in explaining the treatment planning process to patients.
In collaboration with the rest of the medical team, they can help answer patient questions about how the radiation dose is calculated and how the plan aims to protect healthy organs. By contributing their expertise to patient understanding, dosimetrists help foster confidence and address concerns about the technical aspects of radiation therapy. Their careful work ensures that the treatment process, while complex, is designed with the individual patient’s safety and well-being as the top priority.
Dosimetrists assist in patient education, fostering an understanding of the therapy process. (See role aspects on Indeed Career Guide) They play a behind-the-scenes role that significantly impacts patient care. (Read about their impact via Sharp Health News).
The Specifics of a Treatment Planning Dosimetrist
A treatment planning dosimetrist has a range of detailed responsibilities that are crucial for the delivery of safe and effective radiation therapy. A key task involves carefully analyzing various imaging scans, such as CT, MRI, and PET scans. These images help them visualize the patient’s internal anatomy in three dimensions, allowing them to accurately identify the precise location, size, and shape of the tumour, as well as the surrounding healthy organs and sensitive structures that must be avoided.
Based on this anatomical information and the radiation oncologist’s prescription, the dosimetrist performs complex dose calculations using specialized medical dosimetry software. They determine the appropriate type of radiation energy, the number of radiation beams, the angles from which the beams will enter the body, and shape of each beam to conform tightly to the tumour volume. They often conduct treatment simulations on the computer, modeling different scenarios to optimize the dose distribution – maximizing the dose to the cancer target while minimizing exposure to healthy tissues.
Part of their role may also involve testing and calibrating the treatment planning software and participating in quality assurance checks for the radiation delivery equipment. This ensures that the technical aspects of the treatment are accurate and reliable before any radiation is delivered to the patient. Their meticulous work aims for the best possible therapeutic outcome.
Tasks include analyzing imaging scans and conducting simulations to ensure precise treatment. (See task breakdown at Ironwood Cancer & Research Centers).
The job of a treatment planning dosimetrist relies heavily on sophisticated technology and specialized tools. Central to their workflow is advanced treatment planning system (TPS) software. Common examples include systems like Eclipse or Pinnacle. These powerful computer programs allow dosimetrists to import patient imaging data, contour or outline the tumour and critical normal structures, design radiation beam arrangements, calculate dose distributions, and evaluate the quality of the treatment plan.
These systems utilize complex algorithms based on radiation physics to predict how the radiation will interact with the patient’s tissues. Dosimetrists use the software’s 3D modeling and visualization capabilities to refine the plan, ensuring optimal coverage of the target volume while respecting the dose limits for nearby organs. They must be highly proficient in using these intricate software tools and stay updated on the latest technological advancements in imaging and treatment planning to ensure they are leveraging the best available methods for patient care.
Advanced software allows dosimetrists to design precise 3D radiation treatment models. (Visualize the process with the Medical Dosimetrist Overview on YouTube) They utilize the latest technologies to optimize treatment efficacy. (Read about tech use via Sharp Health News).
Ensuring patient safety and treatment effectiveness is paramount in the work of a treatment planning dosimetrist. They are responsible for implementing rigorous safety protocols throughout the planning process. This includes double-checking all calculations, verifying patient data, and ensuring the plan adheres to established clinical guidelines and dose constraints for critical organs. Their expertise in medical dosimetry is crucial for radiation safety.
Before a treatment plan is finalized and approved for delivery, it typically undergoes several layers of review. The dosimetrist presents the plan to the radiation oncologist for clinical approval. It is also reviewed by a medical physicist to ensure its technical accuracy and feasibility. This comprehensive quality assurance process helps catch potential errors and ensures that the final plan is both safe and likely to be effective. By meticulously crafting and verifying each treatment plan, dosimetrists play a vital role in minimizing the risks associated with radiation therapy and maximizing the potential benefits for the patient.
Dosimetrists employ rigorous safety protocols to ensure accurate dose delivery. (Learn about safety focus from Trusted Health) They play a crucial role in radiation safety and effectiveness. (Understand their role in safety from the American Association of Medical Dosimetrists).
Exploring the Field of Medical Dosimetry
The field of medical dosimetry is a specialized area within radiation oncology focused on the measurement and calculation of radiation doses for cancer treatment. It has grown significantly alongside advances in medical imaging and radiation delivery technologies. Decades ago, treatment planning was often simpler, relying on 2D imaging and manual calculations. Today, with technologies like Intensity-Modulated Radiation Therapy (IMRT), Volumetric Modulated Arc Therapy (VMAT), Stereotactic Body Radiation Therapy (SBRT), and proton therapy, the ability to shape and control radiation beams is incredibly sophisticated.
This increasing complexity makes the role of the medical dosimetrist more critical than ever. They are the experts who understand how to harness these powerful technologies safely and effectively. Their detailed knowledge of radiation physics, anatomy, and treatment planning principles allows cancer centers to offer high-precision radiation treatments. The evolution of medical dosimetry reflects the broader progress in oncology, constantly seeking ways to improve cancer control while reducing treatment-related side effects through more targeted therapies.
Medical dosimetry has evolved with advancements in imaging and radiation technologies. (Read about the field’s evolution on the Beekley Blog).
A career in medical dosimetry offers various opportunities for those interested in a blend of science, technology, and patient care. Most certified medical dosimetrists (CMDs) work in clinical settings, such as hospitals and cancer centers, where they are directly involved in patient treatment planning. However, career paths can also lead to roles in research, helping to develop and test new radiation therapy techniques or software. Others might work for medical equipment or software companies, providing training and support to clinical users.
Experienced dosimetrists can also move into educational roles, training the next generation of treatment planning dosimetrist professionals in academic programs. There are opportunities for advancement within clinical departments, potentially leading to supervisory or management positions overseeing the dosimetry team. Many dosimetrists pursue ongoing education and advanced certifications to specialize further or enhance their leadership skills within the field of medical dosimetry.
Career paths include roles in clinical practice, research, and education. (See career options at HealthcareDegree.com) Many dosimetrists pursue advanced certifications and leadership roles. (Explore advancement on Indeed Career Guide).
The meticulous work performed within medical dosimetry has a direct and significant impact on patient outcomes. Accurate dose calculation and precise treatment planning are fundamental to the success of radiation therapy. By ensuring the radiation dose is concentrated effectively within the tumour volume, dosimetrists enhance the likelihood of controlling or eradicating the cancer. Clinical research often relies on accurate dosimetry data to evaluate treatment effectiveness.
Equally important is their role of a dosimetrist in cancer treatment in minimizing the radiation dose delivered to surrounding healthy tissues and critical organs. This careful planning helps reduce the potential for short-term and long-term side effects, improving the patient’s quality of life during and after treatment. In essence, the expertise of medical dosimetrists contributes directly to maximizing the therapeutic benefits of radiation while minimizing its potential harms, making them indispensable contributors to positive patient outcomes.
Dosimetrists significantly improve treatment success rates. (Learn how via Sharp Health News) Their meticulous planning is at the heart of effective cancer treatment. (Understand their central role from the Beekley Blog).
Understanding Dosimetrist vs Radiation Therapist Roles
It’s common for people to confuse the roles of a dosimetrist and a radiation therapist, as both are essential members of the radiation oncology team. However, their responsibilities are distinct. The main difference in the dosimetrist vs radiation therapist comparison lies in their primary function: the dosimetrist designs the treatment plan, while the radiation therapist implements it.
A dosimetrist focuses on the *planning* phase. They work primarily with computers and imaging data to calculate radiation doses and create the detailed map that guides the treatment. Their work requires advanced knowledge of physics, anatomy, and medical dosimetry principles. They typically have limited direct patient contact, working mostly behind the scenes.
In contrast, a radiation therapist is responsible for the *delivery* of the radiation treatment. They operate the linear accelerators or other radiation-emitting machines, position the patient correctly for each session, and administer the radiation dose according to the dosimetrist’s approved plan. Radiation therapists have significant direct interaction with patients daily throughout their course of treatment, providing support and monitoring their condition.
Dosimetrists design treatment plans, while radiation therapists execute them. (See the distinction from the American Association of Medical Dosimetrists) Both roles collaborate closely to provide comprehensive cancer care. (Learn about collaboration at Ironwood Cancer & Research Centers).
The educational pathways and required skill sets also differ between a dosimetrist and a radiation therapist. As mentioned earlier, becoming a dosimetrist typically involves a bachelor’s degree followed by a specialized graduate certificate or master’s program in medical dosimetry, culminating in certification (CMD). Their training heavily emphasizes advanced mathematics, radiation physics, anatomy using medical images, and complex treatment planning software.
Radiation therapists, on the other hand, usually complete an associate’s or bachelor’s degree program specifically in radiation therapy. Their education focuses on patient care, radiation safety procedures, operation of treatment equipment, patient positioning techniques, and basic medical imaging. They must also pass a certification exam administered by the American Registry of Radiologic Technologists (ARRT) to become registered radiation therapists (RTTs). While both roles require technical proficiency and attention to detail, the dosimetrist’s focus is analytical and plan-oriented, whereas the therapist’s is procedural and patient-facing.
Despite their different roles and training, the collaboration between dosimetrists and radiation therapists is essential for high-quality patient care. The dosimetrist vs radiation therapist distinction highlights specialized functions, but their work is interconnected. The dosimetrist creates the blueprint (the treatment plan), and the radiation therapist expertly follows that blueprint to build the structure (deliver the treatment). Therapists provide valuable feedback to dosimetrists, perhaps noting patient setup challenges or changes in anatomy observed during treatment, which might prompt a plan review or adjustment. This teamwork ensures that the high-tech, complex plans created by dosimetrists are translated into safe and accurate treatments delivered with care by the radiation therapists.
Conclusion: The Indispensable Dosimetrist
In summary, understanding what is a dosimetrist reveals a highly specialized and vital professional within the cancer care team. Their expertise in medical dosimetry—the precise calculation and planning of radiation doses—is fundamental to modern radiation oncology. The role of a dosimetrist in cancer treatment involves using advanced technology and a deep understanding of physics and anatomy to design individualized treatment plans that maximize the attack on cancerous tumours while carefully protecting healthy tissues.
The contribution of dosimetrists directly impacts patient safety and the potential effectiveness of radiation therapy. Their meticulous attention to detail ensures that complex treatments are planned accurately, forming the crucial foundation upon which safe treatment delivery rests. Appreciating the technical skill and critical thinking involved in their work helps highlight the sophistication of modern cancer care.
For patients undergoing radiation therapy, knowing that a dedicated expert has carefully crafted their treatment plan can provide reassurance. For those considering careers in healthcare, the field of medical dosimetry offers a rewarding path combining technology, science, and a profound impact on patient lives. The treatment planning dosimetrist is truly an indispensable figure in the fight against cancer.
Dosimetrists are indispensable in the field of cancer treatment, ensuring precision and safety in radiation therapy. (Reaffirm their importance via Trusted Health) Understanding their role is crucial for those undergoing radiation therapy and for individuals considering a career in this rewarding field. (Learn more about the career from the American Association of Medical Dosimetrists).