Estimated Reading Time ~9 minutes
Key Takeaways
- Medical Physicist Definition: Healthcare professionals applying physics principles to medicine, especially in radiation oncology and imaging, ensuring safety and efficacy.
- Education: Requires advanced degrees (Master’s/Ph.D.) in medical physics or related fields, followed by clinical residency training.
- Core Responsibilities: Treatment planning, quality assurance (QA) of equipment, radiation safety expertise, image analysis, research, and collaboration with healthcare teams.
- Proton Therapy Role: Crucial for complex treatment planning, precise dose calculation/delivery, and maintaining sophisticated proton therapy equipment.
- Safety Guardians: Implement safety protocols, ensure regulatory compliance, and manage radiation risks.
- Team Integrators: Essential collaborators in cancer treatment teams, working with oncologists and using advanced imaging for precision care.
Table of Contents
- What Is a Medical Physicist? Definition, Education, and Key Roles
- The Special Role of Medical Physicists in Proton Therapy
- Medical Physicists: Guardians of Safety as Radiation Safety Experts
- The Essential Role of Physicists in Cancer Treatment Teams
- Quality Assurance (QA): Ensuring Precision in Proton Therapy
- Conclusion: The Vital Role of the Medical Physicist
- Frequently Asked Questions (FAQ)
Have you ever wondered about the experts behind the scenes who make advanced medical treatments like radiation therapy possible and safe? Among these vital professionals are medical physicists. So, what is a medical physicist? They are special healthcare professionals who use their knowledge of physics—the science of matter and energy—to help in medicine. They act as a bridge, connecting the world of physics with the needs of doctors and patients.
Medical physicists play a huge part in today’s healthcare, especially in treating cancer with radiation. Think of them as the technical experts who understand how radiation works and how to use it safely and effectively. They make sure the powerful machines used in treatments like proton therapy deliver radiation precisely to the cancer, while protecting the healthy parts of the body as much as possible. This makes them key radiation safety experts. Their careful work is essential for making sure treatments are successful and patients are kept safe. The role of a physicist in cancer treatment is critical. This post will explore more about what medical physicists do, focusing on their important job in proton therapy treatments and overall cancer care.
What Is a Medical Physicist? Definition, Education, and Key Roles
Let’s dive deeper into what is a medical physicist. These professionals are highly trained experts who apply the rules and methods of physics to healthcare. Their main focus is often on how radiation and technology are used to find and treat diseases, particularly cancer. Medical physicists work with complex medical equipment, like imaging machines and radiation therapy units, ensuring they work correctly and safely. They are problem-solvers who use science to improve patient health.
Medical physicists are essential members of the healthcare team. They might not always be seen by patients, but their work behind the scenes is vital. They help doctors plan treatments, make sure equipment is safe, and contribute to developing new medical technologies. Their expertise is especially critical in fields that use complex radiation technology, such as radiation oncology (cancer treatment using radiation) and diagnostic imaging (like X-rays, CT scans, and MRI). According to research, “Medical physicists are specialized healthcare professionals who apply principles and techniques from physics to the prevention, diagnosis, and treatment of human diseases.” Their knowledge is especially needed “in areas that require sophisticated use of radiation and advanced technology.” They are truly “Essential contributors to modern healthcare teams—especially in cancer therapy settings like radiation and proton therapy.”
Becoming a Medical Physicist: Education and Training
Becoming a medical physicist requires a lot of education and specialized training. It’s not a job you can step into right after high school. Most medical physicists have advanced degrees, meaning they’ve gone to university for many years after their initial degree. They usually earn a Master’s degree or a Doctorate (Ph.D.) in medical physics, physics, or a closely related science field like engineering.
After finishing their university studies, they need practical, hands-on training in a hospital or clinic setting. This is often done through a residency program, which is like an apprenticeship where they learn the job under the supervision of experienced medical physicists. These residency programs usually last two or three years and must meet specific standards set by professional organizations. During residency, they learn how to apply their physics knowledge to real patient situations, operate complex equipment, and work as part of the healthcare team. Some medical physicists choose to become certified by passing special exams, which shows they have reached a high level of skill and knowledge in their specialty area, such as radiation therapy physics or imaging physics. As one source notes, “Medical physicists typically hold advanced degrees (such as a master’s or doctorate) in medical physics or a related field, followed by rigorous clinical training. They are trained to practice independently in one or more specialties of medical physics.”
What Does a Medical Physicist Do? Key Responsibilities
The job of a medical physicist involves many important tasks, all focused on using physics principles safely and effectively in medicine. Their responsibilities require deep technical knowledge and strong teamwork skills. Here are some of the main things a physicist in cancer treatment and other areas does:
- Planning and Improving Radiation Treatments: A huge part of their job, especially in cancer care, is designing radiation treatment plans. They work with doctors to figure out the best way to aim radiation at a tumor to destroy cancer cells while protecting the healthy tissues nearby. They use special computer software to calculate the exact dose and path of the radiation beams. This involves “planning and optimizing radiation treatments for patients.”
- Looking at Medical Pictures and Data: Medical physicists help analyze images from machines like CT scanners, MRI machines, and PET scanners. These pictures help doctors see inside the body to diagnose problems and plan treatments accurately. Physicists ensure these images are high quality and sometimes help combine images from different machines for a clearer picture.
- Helping Design Medical Machines: Some medical physicists work on creating or improving medical equipment. They use their physics knowledge to help design safer, more effective machines for diagnosis and treatment. They also test new equipment to make sure it meets safety and performance standards.
- Giving Advice on Radiation Safety: Medical physicists are the go-to radiation safety experts in a hospital or clinic. They develop safety rules and procedures to protect patients, staff, and the public from unnecessary radiation. They monitor radiation levels and make sure the facility follows all safety regulations. This includes “providing expert advice on radiation protection and safety.”
- Teaching and Training: They often teach doctors, medical students, radiation therapists (the people who operate the treatment machines), and other healthcare workers about the physics behind medical technologies and how to use them safely.
- Running Quality Checks (Quality Assurance): Medical physicists are in charge of quality assurance (QA) programs for radiation equipment. This means they regularly test and check the machines to make sure they are working perfectly and delivering the correct amount of radiation exactly where it’s needed. This ensures treatments are both safe and effective.
- Doing Research: Many medical physicists are involved in research. They work to develop new and better ways to use physics in medicine, improve existing treatments, and find innovative solutions to healthcare challenges. Their research helps advance the field and ultimately improves patient care.
Collaboration is key to their success. They don’t work alone; they are part of a large team. “Collaboration is at the heart of their role—they work closely with physicians, nurses, technologists, and patients to ensure the safe and effective use of radiation in medicine.” Their teamwork ensures that complex technologies are used properly for the best patient outcomes.
[Sources for this section:] (Source), (Source), (Source)
The Special Role of Medical Physicists in Proton Therapy
Proton therapy is a very advanced type of radiation treatment used to fight cancer. Unlike traditional radiation therapy that uses X-rays (which are beams of energy like light, but invisible and more powerful), proton therapy uses protons. Protons are tiny particles found in the center of atoms. They have a special property that makes them very useful for treating cancer.
Protons can be aimed very precisely at a tumor. The special thing about protons is that they release most of their energy right at the end of their path and then stop. This allows doctors to deliver a powerful dose of radiation directly to the tumor while reducing the radiation dose to the healthy tissues surrounding and behind the tumor. This precision can be particularly important for certain types of cancer. The medical physicist’s role in the proton therapy planning process is absolutely essential to harnessing this unique property safely and effectively.
Specific Responsibilities in Proton Therapy
Treatment Planning in Proton Therapy:
Creating a proton therapy plan is a highly complex task where the medical physicist plays a leading role. They start by using detailed pictures of the patient’s body, usually from CT scans and sometimes MRI scans, to build a 3D computer model of the tumor and the nearby healthy organs. Using special software, the physicist then calculates the best angles and energies for the proton beams to enter the body and hit the tumor precisely. They carefully shape the radiation dose so that it covers the entire tumor volume while avoiding sensitive healthy structures as much as possible. This involves intricate calculations to account for how protons interact with different body tissues. A key part of their job is to “design individualized proton therapy plans, tailoring dose distributions to achieve optimal tumor coverage while sparing normal tissue.” This ensures each patient gets a plan customized just for them.
Calculating and Delivering the Proton Dose:
Once the plan is designed, the medical physicist must ensure the calculated radiation dose is accurate and that the proton therapy machine can deliver it exactly as planned. Protons behave differently than X-rays, so the dose calculations are very complex, needing advanced computer systems and a deep understanding of proton physics. The physicist verifies that the planned dose matches the tumor’s shape and location perfectly. During the actual treatment sessions, they oversee the setup and delivery. They work closely with the radiation therapists to position the patient correctly and ensure the machine operates flawlessly. Their oversight guarantees that the carefully planned dose is delivered accurately, which is vital for the treatment’s effectiveness and the patient’s safety. As noted in research, “They are responsible for precise dose calculations and ensuring accurate delivery, directly impacting treatment efficacy and patient safety.”
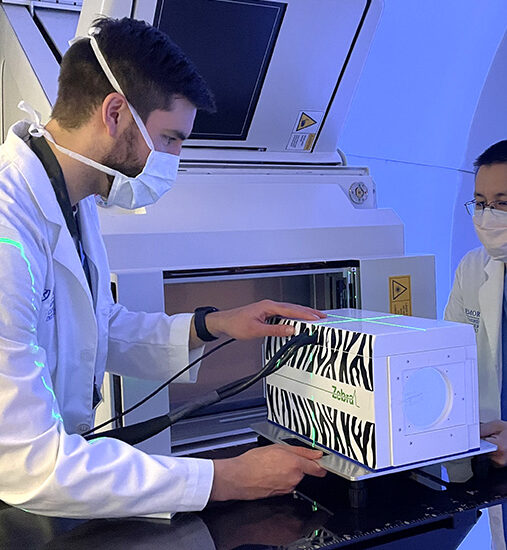
Maintaining the Proton Therapy Equipment:
Proton therapy facilities house massive, complex machines, often involving particle accelerators like cyclotrons or synchrotrons to produce and direct the proton beams. Keeping this sophisticated equipment working perfectly is another crucial job for the medical physicist. They are responsible for the regular checking and calibration of the machines. Calibration means adjusting the machine to make sure it’s delivering the right amount of energy and aiming the beam correctly. They perform daily, weekly, and monthly tests as part of a strict quality assurance (QA) process in proton therapy program. If any technical problems arise, they troubleshoot and work with engineers and service technicians to fix them quickly. They also help implement upgrades or new technologies for the equipment, such as pencil beam scanning technology. Reliable machine performance is critical for patient safety and treatment accuracy, and “Medical physicists routinely calibrate and maintain proton therapy machines, ensuring their reliability and accuracy.” Without their constant vigilance, proton therapy couldn’t be delivered safely or effectively.
The physicist in cancer treatment, especially in the advanced area of proton therapy, carries immense responsibility. Their expertise ensures that this powerful technology is used to its full potential to help patients while minimizing risks.
Medical Physicists: Guardians of Safety as Radiation Safety Experts
Using radiation in medicine, whether for taking pictures like X-rays or for treating cancer, requires extreme care. Radiation can be harmful if not used correctly. This is where medical physicists step in as dedicated radiation safety experts. Their role is to make sure that radiation is used in a way that maximizes the benefit to patients while minimizing any potential risks to patients, hospital staff, and the public.
Making Sure Safety Rules Are Followed:
Medical physicists are responsible for creating and overseeing safety rules, often called protocols, for using radiation in the hospital or clinic. These rules cover everything from how equipment should be operated to how staff should protect themselves and patients from unnecessary radiation exposure. They conduct regular checks, called safety audits, on rooms where radiation is used and on the equipment itself to make sure everything meets high safety standards. Part of their job includes monitoring the levels of radiation in different areas of the facility to ensure they stay well below the limits set by safety regulations. The goal is always prevention – “Medical physicists implement and monitor strict safety protocols to prevent unnecessary radiation exposure for both patients and staff.”
Meeting Government Rules (Regulatory Compliance):
The use of radiation in medicine is strictly controlled by government agencies and international organizations. There are many laws and guidelines that hospitals must follow to ensure safety. Medical physicists are responsible for making sure that all practices involving radiation meet these requirements. This involves keeping detailed records of equipment checks, radiation doses given to patients, and safety procedures. They stay informed about any changes in the laws or guidelines and make sure the hospital updates its practices accordingly. This ensures the facility operates legally and safely, as “They ensure all practices adhere to national and international radiation safety regulations and guidelines.”
Finding and Managing Radiation Risks:
Part of being a radiation safety expert is looking for potential hazards related to radiation use and finding ways to reduce those risks. Medical physicists perform thorough risk assessments. This means they think about what could potentially go wrong in different situations involving radiation and figure out how likely it is to happen and what the consequences might be. Based on these assessments, they develop plans and strategies to minimize these risks. For example, they might recommend changes to how procedures are done, suggest using protective shielding, or implement new safety checks. They also play a key role in educating hospital staff about radiation safety practices and what to do in case of an emergency involving radiation. They work constantly to “assess and mitigate risks associated with radiation use, developing strategies to address any identified hazards.” Their proactive approach is vital for maintaining a safe environment, especially in complex areas like the medical physicist role in proton therapy planning where high-energy radiation is used.
The Essential Role of Physicists in Cancer Treatment Teams
Treating cancer, especially with radiation, is a team effort involving many different healthcare professionals. The physicist in cancer treatment is a core member of this team, bringing unique scientific and technical expertise that is vital for planning and delivering effective care. Their work ensures that radiation therapy is not only powerful against cancer but also precisely targeted and safe.
Working Together on Treatment Plans:
Medical physicists collaborate very closely with radiation oncologists (doctors who specialize in treating cancer with radiation) and other specialists like surgeons and medical oncologists (doctors who treat cancer with medicine). When a patient needs radiation therapy, the physicist works side-by-side with the radiation oncologist to develop the best possible treatment plan. The oncologist decides the overall strategy and the dose of radiation needed, while the physicist figures out the technical details – how to deliver that dose accurately to the tumor while protecting nearby healthy organs. They provide crucial insights into beam arrangements, energy selection (especially important in the medical physicist role in proton therapy planning), and dose calculations. They regularly participate in team meetings where different specialists discuss patient cases and coordinate care, ensuring everyone is on the same page. This teamwork is essential, as “Medical physicists work side-by-side with oncologists and other specialists to create comprehensive, effective cancer treatment plans.”
Using Advanced Imaging for Precision:
Modern radiation therapy relies heavily on advanced imaging technologies to see the tumor and surrounding tissues clearly. Medical physicists are experts in using and interpreting images from CT (Computed Tomography), MRI (Magnetic Resonance Imaging), and PET (Positron Emission Tomography) scans. These images are used to precisely map the location, size, and shape of the tumor. Physicists often use sophisticated computer techniques to combine, or ‘fuse,’ images from different types of scans. This image fusion gives the treatment planning team the clearest possible view, allowing for incredibly accurate targeting of the radiation beams. During the course of treatment, new images might be taken to see if the tumor is shrinking or if anything has changed. Physicists analyze these images to help the team monitor progress and make any necessary adjustments to the treatment plan. Their skills ensure that treatments remain accurate even if changes occur, as “They utilize and interpret advanced imaging technology to accurately locate tumors, monitor progress, and refine treatments.”
Driving Research and Innovation:
Medical physicists are not just users of technology; they are often involved in developing and improving it. Many are actively engaged in research to find new and better ways to use radiation against cancer. This might involve developing new treatment techniques, improving imaging methods, refining dose calculation algorithms, or exploring entirely new types of radiation or equipment. They often participate in clinical trials, which are research studies that test new treatments on patients to see if they are safe and effective. By conducting research, publishing their findings in scientific journals, and sharing knowledge with colleagues around the world, medical physicists contribute significantly to advancing the field of cancer treatment. Their goal is always to find ways to make treatments more effective, reduce side effects, and improve outcomes for patients.
Quality Assurance (QA): Ensuring Precision in Proton Therapy
Proton therapy offers a highly precise way to target cancer, but this precision relies completely on the equipment working perfectly every single time. Ensuring this level of accuracy and consistency is the job of Quality Assurance, or QA. Medical physicists are responsible for designing and running comprehensive QA in proton therapy programs. This involves constant checking and testing to make sure every aspect of the treatment is safe and accurate.
Regular Checks and Tests (Routine QA Procedures):
The complex machines used for proton therapy need careful monitoring. Medical physicists establish schedules for routine checks – some tests are done every day before treatments begin, others weekly, monthly, or annually. These tests check critical aspects of the machine’s performance, such as the energy of the proton beam, the accuracy of the beam’s position and shape, the function of the imaging systems used for patient positioning, and the safety systems that protect patients and staff. They use specialized measurement tools, called phantoms and detectors, to simulate patient treatments and verify that the radiation dose delivered matches exactly what was planned. These routine checks confirm that the equipment is performing within very tight tolerances, ensuring consistent and reliable treatment delivery day after day. This involves “regular testing and validation of proton therapy equipment to maintain high treatment standards.”
Finding and Fixing Problems (Error Detection and Correction):
Even with the best equipment, things can sometimes go wrong. A crucial part of QA in proton therapy is having systems in place to detect any errors or deviations from the expected performance as quickly as possible. Medical physicists analyze the data collected during routine QA tests to spot any trends or small changes that might signal a developing problem. They also investigate any errors that might occur during treatment delivery. If a problem is found, whether it’s a small machine malfunction or a discrepancy in the delivered dose, they work with engineers and the clinical team to understand the cause and fix it immediately. They establish procedures for investigating incidents and making sure corrections are properly implemented and documented. This system of checks and balances helps maintain the highest standards of safety and accuracy.
Always Getting Better (Continuous Improvement):
Quality assurance isn’t just about fixing problems; it’s also about constantly looking for ways to make things even better. Medical physicists involved in QA in proton therapy are committed to continuous improvement. They stay updated on the latest technological advancements and research findings in medical physics and proton therapy. They use feedback from the clinical team and data from ongoing monitoring to refine QA procedures and treatment processes. For example, they might implement new testing methods that provide more detailed information about beam quality or adopt new software tools that improve the accuracy of dose verification. This dedication to ongoing enhancement ensures that the proton therapy program not only meets current standards but also strives for excellence, incorporating the best available practices to improve treatment precision and effectiveness. The medical physicist role in proton therapy planning includes engaging in these ongoing quality improvement efforts.
Conclusion: The Vital Role of the Medical Physicist
So, what is a medical physicist? As we’ve explored, they are highly skilled healthcare professionals who blend the principles of physics with the practice of medicine. Their work is absolutely essential for the safe and effective use of radiation in diagnosing and treating diseases, particularly cancer. They are the invisible experts ensuring that complex technologies work precisely as intended.
The medical physicist role in proton therapy treatments highlights their importance in cutting-edge treatments. They meticulously plan treatments, calculate precise doses, and ensure the sophisticated equipment delivers radiation accurately, maximizing the impact on tumors while protecting healthy tissues. Their role as radiation safety experts is paramount, implementing protocols and checks that safeguard both patients and healthcare workers. Furthermore, their commitment to rigorous quality assurance (QA) in proton therapy guarantees the reliability and accuracy needed for such advanced procedures.
Working closely with doctors and other healthcare professionals, the physicist in cancer treatment is a key player in the multidisciplinary team. They contribute technical expertise, support advanced imaging, and drive research to continually improve care. Their dedication ensures that patients receive the benefits of powerful radiation therapies safely and effectively. The next time you hear about advanced cancer treatments like proton therapy, remember the medical physicists working diligently behind the scenes. Their unique skills and commitment are fundamental to successful patient outcomes and the ongoing advancement of medical science.
Frequently Asked Questions (FAQ)
Q1: What is the difference between a medical physicist and a doctor (radiation oncologist)?
A1: A radiation oncologist is a medical doctor who prescribes radiation therapy and manages the overall patient care. A medical physicist is a scientist with expertise in physics who focuses on the technical aspects of radiation delivery, treatment planning, equipment calibration, quality assurance, and radiation safety. They work together as part of the treatment team.
Q2: Are medical physicists only involved in cancer treatment?
A2: While many medical physicists specialize in radiation oncology (cancer treatment), others work in diagnostic imaging (like X-ray, CT, MRI, nuclear medicine), ensuring image quality and radiation safety, or in nuclear medicine physics, dealing with radioactive materials for diagnosis and therapy. Some are also involved in research and development of new medical technologies.
Q3: Do patients meet the medical physicist during proton therapy?
A3: Patients might not always directly interact with the medical physicist, as much of their work happens behind the scenes (treatment planning, QA checks). However, they are a critical part of the care team ensuring the safety and accuracy of the treatment. In some situations, such as complex setups or specific procedures, the physicist might be present in the treatment room or involved in patient consultations.
Q4: Why is quality assurance (QA) so important in proton therapy?
A4: Proton therapy relies on delivering highly focused radiation beams precisely to the tumor. Even small errors in beam energy, position, or dose calculation can significantly impact treatment effectiveness and potentially harm healthy tissues. Rigorous QA, overseen by medical physicists, ensures the complex equipment functions perfectly and the treatment is delivered exactly as planned, maximizing safety and the chances of success.