Estimated Reading Time: 12 minutes
Key Takeaways
- Proton Therapy Basics: Proton therapy is a specialized radiation treatment using proton beams that stop at the tumor site (the Bragg Peak), minimizing damage to surrounding healthy tissue.
- Pencil Beam Scanning (PBS) Defined: PBS is the most advanced method for delivering proton therapy, using a narrow, magnetically guided proton beam to precisely “paint” the tumor volume spot by spot, layer by layer.
- Enhanced Precision: PBS and related proton therapy precision techniques allow for highly conformal dose distributions, tightly matching complex tumor shapes, particularly near critical organs.
- Intensity-Modulated Proton Therapy (IMPT): An even more refined technique built on PBS, IMPT technology modulates the intensity of the proton beam at each spot, offering superior dose control for intricate cases.
- Patient Benefits: Advanced delivery methods like PBS aim to improve tumor control while reducing side effects, leading to better patient quality of life during and after treatment.
Table of Contents
- Understanding Advanced Proton Therapy
- Exploring Advanced Proton Therapy Techniques
- What is Pencil Beam Scanning?
- Pencil Beam Scanning in Proton Therapy Application
- Examining Proton Therapy Precision Techniques
- IMPT Technology in Detail
- Benefits of Advanced Delivery Systems in Proton Therapy
- The Future of Advanced Proton Therapy
- Conclusion
- Frequently Asked Questions (FAQ)
- Resources and Further Reading
- Previous Blog Posts
Cancer treatment has seen incredible advancements, and one of the most revolutionary forms is proton therapy. This type of radiation therapy uses protons, which are tiny parts of atoms with a positive charge, to very carefully target and treat cancerous cells. A key benefit of this advanced treatment is its ability to minimize harm to the healthy tissues surrounding a tumor, which is often a challenge with older forms of radiation. Within the field of proton therapy, technology continues to evolve, leading to even greater accuracy. So, what is pencil beam scanning? It’s a highly advanced delivery method used in proton therapy today. Pencil beam scanning (PBS) uses an extremely narrow proton beam, about the width of a pencil lead, to precisely “paint” the tumor with radiation, one spot at a time. This technique represents a major step forward in proton therapy precision techniques, making treatment potentially more effective while protecting the patient’s healthy body parts. This article will delve into how pencil beam scanning works, its advantages, and its important role in advanced proton therapy for modern cancer care. We aim to explain the mechanisms, benefits, and future possibilities of this cutting-edge technology, showing how precision is improving cancer treatment. Proton therapy itself is transforming cancer care by delivering radiation with high accuracy, reducing damage to healthy areas.
Understanding Advanced Proton Therapy
Let’s start with the basics. What is proton therapy? It’s a specialized kind of radiation treatment that uses beams of protons directed at cancerous tumors. Protons are accelerated to very high speeds, giving them enough energy to travel deep into the body to reach the tumor site. The way proton therapy works is quite different from traditional radiation therapy, which typically uses X-rays (also called photons). Traditional X-ray beams release energy continuously as they travel through the body, meaning they affect both the tumor and the healthy tissues they pass through on their way in and out. This is not necessarily bad for most cancer types, but in certain situations, proton therapy’s advantages make sense for the patient and their disease.
Proton therapy takes advantage of a unique physical property known as the “Bragg Peak“. This phenomenon means that protons release the vast majority of their energy at a very specific depth inside the body—right where the tumor is located. After hitting their target depth, the protons stop, delivering very little radiation dose beyond the tumor. This precise energy deposit is a core reason why advanced proton therapy is considered a major step forward in radiation oncology. It allows doctors to target the cancer cells more effectively while significantly reducing the radiation exposure to nearby healthy organs and tissues. This characteristic makes proton therapy a potentially gentler option, especially for tumors located close to critical body structures.
Exploring Advanced Proton Therapy Techniques
Proton therapy technology hasn’t stood still; it has continually improved over the years with innovations designed to boost its accuracy and effectiveness. While the basic principle of using protons remains the same, the methods for delivering the proton beam have become much more sophisticated. Early methods involved spreading the beam out, but newer advanced proton therapy techniques offer much greater control. Among these innovations, pencil beam scanning (PBS) has risen to prominence and is often considered the most advanced and precise delivery method available today. Other techniques used in proton therapy include passive scattering and uniform scanning, which were important steps but generally offer less conformality than PBS.
The importance of precision in any cancer treatment, especially radiation therapy, cannot be overstated. The primary goal is always to deliver an effective dose of radiation to the cancerous tumor while minimizing exposure and potential harm to the healthy tissues and organs nearby. Precise targeting maximizes the destructive effect on cancer cells and simultaneously helps protect the patient’s healthy body parts from unnecessary radiation damage. This protection is vital for reducing potential side effects, both immediate and long-term, and for maintaining the patient’s quality of life during and after treatment. Precision is particularly critical when dealing with tumors that have irregular shapes or are located adjacent to sensitive structures like the optic nerve, brainstem, or heart. Advanced proton therapy precision techniques, such as pencil beam scanning, are therefore instrumental in achieving the best possible balance between effectively treating the cancer and safeguarding the patient’s overall health and well-being. Achieving optimal treatment outcomes often relies heavily on these sophisticated delivery methods, as highlighted by resources like ITN Online.
What is Pencil Beam Scanning?
So, what is pencil beam scanning exactly? It’s a highly sophisticated method for delivering proton therapy. Instead of using a broad beam of protons that needs to be shaped before it hits the patient, pencil beam scanning (often abbreviated as PBS) uses a very narrow, focused beam of protons – typically just a few millimeters wide, like the tip of a pencil. This fine beam is then used to meticulously “paint” the tumor with radiation, depositing the dose spot by spot, layer by layer. This approach allows for incredible precision in targeting the cancer.
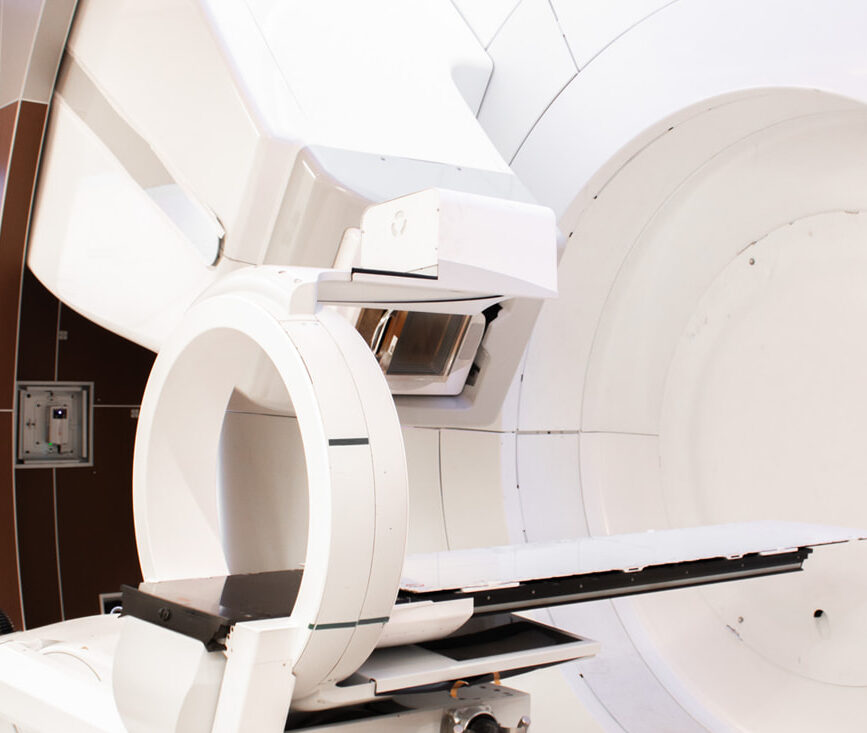
How does pencil beam scanning in proton therapy actually operate? The system uses powerful magnets to precisely steer this narrow proton beam. These magnets can rapidly guide the beam horizontally and vertically across the target area. The energy of the proton beam is also carefully controlled to determine how deep into the tissue the protons travel before depositing their energy (remember the Bragg Peak). By combining this magnetic steering with adjustments to the beam’s energy, PBS can deliver radiation doses that conform very tightly to the three-dimensional shape of the tumor, no matter how complex or irregular it might be. The system adjusts the beam’s intensity (how many protons are delivered to each spot) and its position constantly throughout the treatment session, ensuring the prescribed radiation dose is delivered accurately throughout the entire tumor volume. More details can be found at the Texas Center for Proton Therapy, ProTom International, and ITN Online.
Pencil beam scanning plays a crucial role in modern advanced proton therapy. It is generally considered superior to older methods like passive scattering. Passive scattering required the creation of custom hardware devices (called apertures and compensators) for each patient to shape the beam, which was time-consuming and less precise. PBS eliminates the need for this patient-specific hardware, making treatment planning and delivery potentially more efficient and flexible. Furthermore, pencil beam scanning provides the technological foundation for an even more advanced technique called Intensity-Modulated Proton Therapy (IMPT). IMPT technology builds upon PBS by not only controlling the beam’s position but also modulating, or varying, the intensity of the beam at each individual spot within the tumor. This allows for an even finer level of dose control and sculpting, particularly useful for very complex tumor shapes near sensitive organs. Learn more from ProTom International and Wikipedia’s explanation of PBS.
Compared to traditional radiation methods and older proton techniques, proton therapy precision techniques like PBS offer significant advantages. The most notable is enhanced targeting accuracy. PBS can conform the radiation dose very precisely to complex tumor geometries, even those wrapped around critical structures. This exceptional conformality minimizes the radiation dose delivered to adjacent healthy tissues and organs, reducing the risk of side effects. This improved targeting accuracy directly contributes to potentially better treatment outcomes. By sparing healthy tissue, PBS can lead to fewer immediate and long-term complications from radiation exposure. This precision may also allow oncologists to safely deliver higher, more potent radiation doses directly to the tumor when appropriate, potentially increasing the chances of controlling the cancer. Patients often benefit from potentially shorter treatment setup times and an overall better quality of life during and after their course of therapy due to reduced toxicity, as discussed by the Texas Center for Proton Therapy and ITN Online.
Pencil Beam Scanning in Proton Therapy Application
The implementation of pencil beam scanning in proton therapy is a meticulous process involving several key steps to ensure accuracy and safety. First, detailed Tumor Mapping is performed using advanced imaging technologies like CT (Computed Tomography), MRI (Magnetic Resonance Imaging), and sometimes PET (Positron Emission Tomography) scans. These scans create a precise three-dimensional map of the tumor and the surrounding normal tissues.
Next comes Treatment Planning. A dedicated team of medical physicists, dosimetrists, and radiation oncologists uses specialized computer software to design a personalized treatment plan based on the 3D tumor map. This plan details the exact paths the proton beam should take, the energy levels required to reach different depths within the tumor, and the intensity (dose) needed for each spot to deliver the prescribed radiation effectively while sparing nearby healthy structures.
During the Beam Delivery stage, the patient is carefully positioned on the treatment table. The pencil beam scanning system then executes the treatment plan. Powerful electromagnets guide the narrow proton beam, moving it rapidly across the tumor volume in a pre-programmed pattern, often described as a raster scan (like an old TV drawing a picture line by line). Radiation is delivered spot by spot, and layer by layer, building up the required dose throughout the entire tumor shape. Finally, Dose Verification systems are used throughout the process. Real-time monitoring and imaging techniques are often employed to confirm that the patient is positioned correctly and that the radiation dose is being delivered accurately according to the plan.
The patient benefits associated with proton therapy precision techniques like PBS are significant. Because less radiation hits healthy tissues, patients may experience fewer immediate side effects (like skin irritation, fatigue, or nausea) and may have a lower risk of developing long-term complications years after treatment. Depending on the treatment center’s workflow and the specific case, the efficiency of PBS delivery might contribute to Shorter Treatment Session Times compared to older, hardware-intensive methods, although the overall course of treatment still involves multiple sessions over several weeks.
Examining Proton Therapy Precision Techniques
Pencil Beam Scanning (PBS) stands out as the most sophisticated method among various proton therapy precision techniques, but it’s helpful to understand how it compares to other approaches. Passive Scattering represents an older generation of proton therapy delivery. In this method, a broad proton beam is generated and then spread out or shaped using materials called scattering foils, and patient-specific devices like brass apertures (to shape the beam laterally) and plastic compensators (to shape the dose distally). While effective for many years, passive scattering delivers a more uniform dose across the target and typically requires custom hardware for each patient, adding complexity and time to the treatment preparation process. Uniform Scanning is another technique that uses magnets to scan the proton beam across the tumor, similar to PBS, but it typically delivers a uniform dose layer by layer rather than varying the intensity spot by spot.
Pencil Beam Scanning, in contrast, offers unparalleled precision by actively steering a very fine beam and depositing dose point by point. This active control allows it to conform the dose delivery much more accurately to the intricate shapes of tumors, especially complex ones, thereby maximizing the dose to the cancer while minimizing exposure to surrounding healthy tissues.
Building upon the capabilities of PBS is IMPT Technology. Intensity-Modulated Proton Therapy (IMPT) is arguably the most advanced form of proton therapy delivery currently available. It uses the same pencil beam scanning mechanism to precisely position the beam, but it adds another layer of control: intensity modulation. This means that the intensity, or strength, of the proton beam can be adjusted for every single spot (or voxel) within the tumor target volume. By varying the number of protons delivered to each specific point, IMPT allows clinicians to “sculpt” the radiation dose distribution with extraordinary precision. It enables the creation of highly conformal dose distributions that tightly match complex tumor shapes, even those that are concave or wrap around critical organs. This enhanced control provides superior tumor targeting capabilities while offering the maximum possible sparing of adjacent healthy tissues, potentially leading to improved treatment outcomes and reduced side effects for challenging cancer cases.
IMPT Technology in Detail
Let’s dive deeper into IMPT technology. From a technical standpoint, Intensity-Modulated Proton Therapy relies heavily on sophisticated computer algorithms for treatment planning. This process, often called “inverse planning,” starts with the radiation oncologist defining the target tumor volume and outlining critical nearby healthy organs that need protection. The desired radiation dose for the tumor and the maximum tolerance doses for the healthy organs are specified. Then, powerful computers calculate the optimal combination of proton beam angles, energies, positions, and, crucially, intensities for each spot within the target necessary to achieve the prescribed dose distribution. This complex calculation allows IMPT to create dose patterns that would be impossible with simpler techniques, enabling potential dose escalation within the tumor while strictly adhering to constraints designed to protect sensitive normal tissues.
Compared to other proton therapy precision techniques like passive scattering or uniform scanning, IMPT offers a significantly higher degree of control over the dose distribution. This makes it particularly well-suited for treating cancers with highly irregular shapes or tumors located in anatomically complex areas where critical structures are immediately adjacent to the target volume. The ability to modulate intensity at each point provides the flexibility needed to shape the dose precisely around these sensitive areas.
IMPT technology and pencil beam scanning in proton therapy work together synergistically. PBS provides the fundamental mechanism for precise beam delivery – steering the narrow beam spot by spot. IMPT builds directly upon this foundation by adding the capability to vary the intensity of that beam at each spot. This combination enhances the overall ability to conform the high-dose radiation region tightly to the tumor volume while simultaneously minimizing the dose to surrounding healthy tissues. This optimization of treatment delivery aims to maximize the therapeutic effect on the cancer while reducing the potential for treatment-related side effects, leading to potentially more effective and safer cancer treatments.
The field of advanced proton therapy continues to evolve. Future developments related to IMPT and PBS include advancements in imaging technologies (like cone-beam CT or MRI integrated with the treatment machine) to better visualize the tumor and normal tissues immediately before or even during treatment. This supports the concept of Adaptive Proton Therapy, where treatment plans might be adjusted in real-time or on a daily basis to account for changes in tumor size or patient anatomy during the course of treatment. Ongoing clinical trials are continuously exploring the efficacy of IMPT for various cancer types and comparing its outcomes against other advanced radiation techniques, further refining its role in cancer management.
Benefits of Advanced Delivery Systems in Proton Therapy
The use of advanced delivery systems like Pencil Beam Scanning (PBS) and Intensity-Modulated Proton Therapy (IMPT) in advanced proton therapy offers substantial benefits, primarily centered around enhanced precision and potentially improved patient outcomes. The ability to precisely target the tumor while sparing healthy tissue is key. This Improved Tumor Control stems from the capacity to potentially deliver higher, more effective radiation doses directly to the cancer cells, increasing the likelihood of destroying the tumor. Simultaneously, the sharp dose fall-off characteristic of protons, combined with the accuracy of PBS and IMPT technology, leads to significantly Reduced Side Effects. By minimizing the radiation dose to surrounding healthy organs and tissues, these advanced techniques lower the risk of both short-term complications (like fatigue, nausea, skin reactions) and long-term side effects that could impact organ function years later.
Beyond the direct impact on the tumor, these proton therapy precision techniques contribute positively to the Patient Quality of Life. With potentially fewer and less severe side effects, patients may experience Faster Recovery Times after each treatment session and following the completion of their therapy course. Less toxicity often means patients are better able to Maintain Daily Activities, such as working, spending time with family, and pursuing hobbies, throughout their treatment period. This ability to maintain normalcy can significantly improve a patient’s overall well-being and outlook during a challenging time.
While the initial cost of building and equipping a proton therapy center is high, advanced delivery systems like PBS can offer Cost-Effectiveness in the long run. By reducing treatment-related side effects and complications, there may be Long-Term Savings in healthcare costs associated with managing those side effects. Furthermore, the Efficiency in Treatment Delivery provided by PBS, which eliminates the need for patient-specific hardware used in older techniques like passive scattering, can reduce treatment preparation time and potentially streamline the clinical workflow. This efficiency might contribute to lower operational costs over time compared to less advanced methods.
The Future of Advanced Proton Therapy
The field of advanced proton therapy is dynamic, with ongoing research and development aimed at making the technology even more precise, effective, and accessible. Several emerging technologies promise to shape the future of this treatment modality. One significant trend is the development of Compact Proton Therapy Systems. Traditional proton centers require massive, complex, and expensive equipment. Newer designs focus on smaller footprints, potentially lower costs, and simplified operation, which could make proton therapy available in more hospitals and cancer centers, expanding patient access beyond major metropolitan areas. Another exciting area is the integration of Artificial Intelligence in Treatment Planning. AI algorithms have the potential to analyze complex imaging data and patient information rapidly, helping clinicians create highly optimized and personalized treatment plans even faster and potentially with greater precision than manual methods allow.
Research and Development efforts continue at a brisk pace. Numerous Clinical Trials are underway globally, investigating the use of advanced proton therapy techniques like PBS and IMPT for a wider range of cancer types, comparing their effectiveness against other treatments, and exploring novel combinations with chemotherapy, immunotherapy, and other targeted agents. Technological Innovations are also focusing on improving accelerator technology (the machines that create and speed up the protons) and refining beam delivery systems for even greater speed, accuracy, and real-time adaptation during treatment.
A major goal for the future is Expanding Accessibility of these powerful proton therapy precision techniques. Cost Reduction Efforts are crucial, driven by technological advances like compact systems and potentially more efficient workflows. Increasing the Global Availability by building more proton therapy centers worldwide is essential to reach more patients who could benefit. Finally, persistent advocacy and growing clinical evidence aim to achieve broader Insurance Coverage Expansion, ensuring that these advanced treatments are financially feasible for more patients, regardless of their location or healthcare plan. The future holds promise for making proton therapy a more widespread and standard option in the fight against cancer. Further reading on future directions can be found via sources like ProTom International and ITN Online.
Conclusion
In summary, understanding what is pencil beam scanning reveals it to be a cornerstone of modern, advanced proton therapy. This sophisticated delivery method utilizes a fine proton beam guided by magnets to precisely paint tumors with radiation, offering unmatched accuracy in conforming the dose to the cancer’s shape while sparing surrounding healthy tissues. Building upon this, IMPT Technology further refines proton therapy precision techniques by adding the ability to modulate the intensity of the beam spot by spot, allowing for even greater control, especially for complex cases.
These advanced precision techniques represent significant progress in the field of radiation oncology and cancer treatment overall. They offer the potential for improved tumor control and, very importantly, aim to reduce the side effects associated with treatment by minimizing damage to healthy parts of the body. This provides tangible hope for better outcomes and an enhanced quality of life for many individuals facing a cancer diagnosis.
If you or someone you know is considering cancer treatment options, it’s important to have informed discussions with qualified healthcare professionals. Exploring whether advanced proton therapy, potentially utilizing pencil beam scanning or IMPT, is a suitable option requires consultation with experts in the field. They can assess individual circumstances and help determine the most appropriate, personalized treatment plan based on the specific type and location of the cancer, as well as overall health.
Frequently Asked Questions (FAQ)
How Does Pencil Beam Scanning Differ from Traditional Proton Therapy Methods?
Older proton therapy methods, like passive scattering, used a broad proton beam that had to be shaped using physical devices (apertures and compensators) specific to each patient. Pencil beam scanning (PBS), a key part of advanced proton therapy, uses a very narrow beam that is magnetically steered to “paint” the tumor spot-by-spot and layer-by-layer. This allows for much greater precision and conformality to the tumor shape without needing patient-specific hardware, potentially leading to better sparing of nearby healthy tissues. Understanding what is pencil beam scanning highlights this active, dynamic beam delivery versus older passive shaping methods.
Is Pencil Beam Scanning Suitable for All Types of Cancer?
Pencil beam scanning in proton therapy is particularly beneficial for tumors that are irregularly shaped, located very close to critical or sensitive organs (like the brain, spinal cord, eyes, heart), or where minimizing radiation dose to surrounding healthy tissue is especially important. While it can be used for many types of solid tumors in adults, the decision to use PBS depends on a careful evaluation by the radiation oncology team, considering the tumor type, location, size, and the patient’s overall health. It’s not necessarily required or advantageous for every single case.
What is the Availability of Pencil Beam Scanning?
The availability of pencil beam scanning has been increasing steadily as more proton therapy centers are built worldwide and existing centers upgrade their technology. However, proton therapy, particularly with advanced techniques like PBS and IMPT, is still less widely available than conventional radiation therapy. Most PBS facilities are located at major academic medical centers or specialized cancer treatment hubs like the Tennessee Oncology Proton Center. Patients interested in this technology are encouraged to reach out to our team at the Tennessee Oncology Proton Center.